
Recent Development in Biocompatible Biosensors
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License(https://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The shift in the medical paradigm from treatment to prevention and diagnosis has underscored the growing significance of biosensors. Notably, the recent COVID-19 pandemic has spurred the widespread adoption of biosensors for the detection of viral genes and antigens. Consequently, there has been a substantial increase in both the demand for biosensors and the industries associated with their production. Furthermore, biosensors find applications not only in healthcare but also in diverse fields such as environmental monitoring, food quality control, military defense, and industrial processes. In this brief review, we delve into the essential attributes of biosensors, namely sensitivity, selectivity, and stability. We provide an overview of the latest research trends aimed at improving these attributes. Additionally, we introduce recent research cases in which these attributes are being applied both in vivo and in vitro.
Keywords:
Prevention, Diagnosis, Healthcare, Biosensor, Biomedicine, Pandemic1. INTRODUCTION
Human life expectancy has seen a notable increase in recent years, leading to a growing elderly population worldwide. This demographic shift has sparked significant interest in health and a surging demand for advanced diagnosis of human diseases and personal health management. Consequently, there has been a substantial rise in the demand for biosensors capable of real-time health monitoring and early disease diagnosis. In 2022, the biosensor market was valued at $27.06 billion, and it is projected to sustain an average annual growth rate of 9% through 2026. Biosensors are not limited to healthcare but have also garnered attention in other domains, including medical diagnosis, monitoring, biometric authentication, security, and behavioral pattern analysis feedback. In vivo sensors are designed for direct insertion or attachment to the human body and are primarily utilized in the medical field [1-3]. These sensors proficiently detect and analyze the body's physiological signals, enabling critical functions such as diagnosis, monitoring, and treatment. Notably, in vivo devices like ECG sensors for heart activity and EEG sensors for brain activity are instrumental in diagnosing and studying disorders of the heart and nervous system [4,5]. In contrast, in vitro sensors operate externally and are commonly employed in laboratory settings and medical diagnostic devices. They play a pivotal role in collecting biological samples from external environments, particularly in blood tests to measure parameters like blood sugar levels, blood type, or the presence of infectious disease markers. The evolution of biosensors holds tremendous potential for revolutionizing medical diagnosis and treatment and unlocking new opportunities in the bio industry [6-8]. As our quality of life improves, the demand for biosensors continues to rise, and their applications extend to new fields. Biosensor research has been approached from various angles, including enhancing sensitivity, stability, flexibility, and biodegradability. Enhanced sensitivity enables low-power operation and accurate detection and diagnosis. Improved stability contributes to data reliability, long-term use, and reduced noise and errors. Additionally, increased flexibility allows sensors to respond more robustly to external shocks and establish closer contact with the area being sensed, thus improving sensitivity [9-12]. Biodegradability is a vital characteristic, especially when biosensors are implanted in the body, as it eliminates the need for additional surgery to remove the sensor if it is made from biocompatible materials [13-15]. In this paper, we provide a concise overview of recent advancements in biosensors. We begin by summarizing recent research aimed at enhancing sensor properties and then explore emerging research trends and applications of in vivo and in vitro sensors.
2. Performance Requirements of Biosensor
Considerable research has been dedicated to integrating biosensors into our daily lives, with a focus on enhancing their sensitivity, selectivity, and stability, crucial attributes of biosensors [16-18]. In this section, we provide a summary of recent research aimed at improving these three essential properties.
2.1 Sensitivity
Improving sensitivity in biosensors encompasses various strategies, including the development and utilization of new nanomaterials, bioreceptor advancement, sample preprocessing techniques, and enhancements to device structure. For example, Zhiyong Zhang et al. employed a field-effect transistor-based biosensor for the detection of carcinoembryonic antigen (CEA), a lung cancer biomarker. In this innovative study, a wavy yttrium oxide (Y2O3) dielectric layer was introduced, replacing the conventional flat dielectric layer, to enhance the biosensor's sensitivity. This wavy dielectric layer increased the sensor's capacitance by 50%, resulting in an extended detection range from 1 fg/mL to 1 ng/mL, with an impressive sensitivity of 72 ag/mL. Notably, the sensing platform demonstrated reliability even in the complex environment of fetal bovine serum, holding significant promise for early lung cancer screening (Fig. 1) [19].
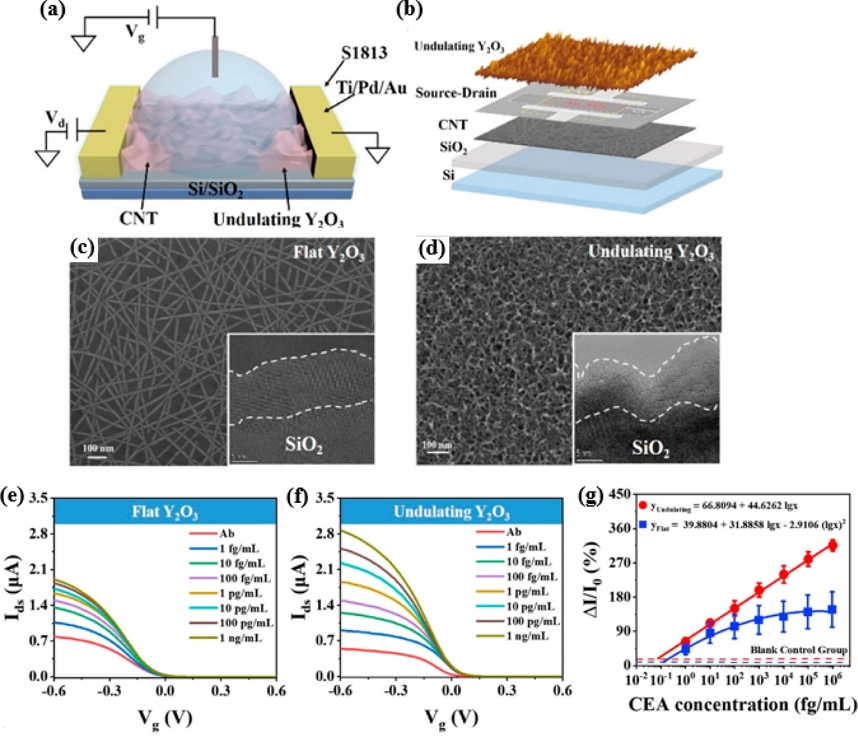
(a) Schematic of three-dimensional undulating FG CNT-FET biosensor. (b) SEM and AFM images of a CNT-FET biosensor with the major sensing regions and morphology of the undulating Y2O3. (c) SEM images of flattened Y2O3 layer. (d) SEM image of undulated Y2O3 layer. (e) Transfer curve evolution of the CNT-FET biosensor with a flat interface, recorded after the introduction of various CEA concentrations ranging from 1 fg/mL to 1 ng/mL. (f) Transfer curve evolution a CNT-FET biosensor with an undulating interface corresponding to different CEA concentrations (0, 1 fg/ mL, 10 fg/mL, 100 fg/mL, 1 pg/ mL, 10 pg/mL, 100 pg/ mL, and 1 ng/mL). (g) Calibration curves of the value (ΔI/I0) vs CEA concentration using proposed FET biosensor with either an undulating interface (red) or flat interface (blue). (Reproduced from [19], with permission from ACS Publications, 2023.)
Sunkook Kim et al. developed a field-effect transistor (FET)-based biosensor for the detection of prostate-specific antigen (PSA), a prostate cancer biomarker. However, the practical application of bio-FETs in this context is often hindered by issues related to reliability and low sensitivity. In their study, they presented a highly sensitive bio-FET by introducing nanoporous molybdenum disulfide (MoS2) and incorporating a non-planar Al2O3 dielectric layer. These modifications reduced hysteresis to a narrow range of 0.44−1.9 V, significantly enhancing accuracy and data reliability. Furthermore, the subthreshold swing (SS) was minimized from 4.06−7.03 V/dec to 1.32−4.67 V/dec, and mobility was increased, resulting in the fabrication of a highly sensitive biosensor with a detection limit of 1 fg/ml. Utilizing this sensor, PSA was successfully and selectively detected in human serum during actual clinical trials, offering the prospect of label-free, rapid prostate cancer detection (Fig. 2) [20].
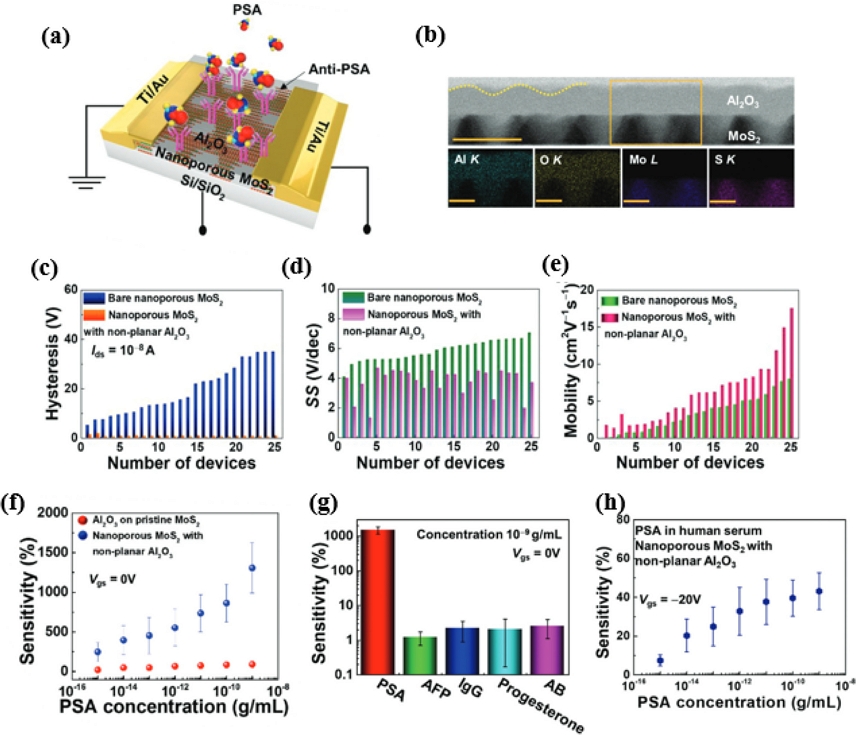
(a) Schematic of concept and morphology of nanoporous MoS2 FETs with non-planar Al2O3 3D schematics of nanoporous MoS2 surrounded by non-planar Al2O3 bio-FET. (b) Cross-sectional STEM micrograph (scale bar 50 nm). Various plots of (c) hysteresis, (d) SS, and (e) mobility of 25 FETs of nanoporous MoS2 FET with non-planar Al2O3 and bare nanoporous MoS2 FET. (f) Comparison of sensitivity (%) as a function of PSA concentration in nanoporous MoS2 bio-FETs with non-planar Al2O3 and planar Al2O3 on pristine MoS2 bio-FETs. (g) Selectivity for detecting PSA for nanoporous MoS2 bio-FETs with non-planar Al2O3 with potentially interfering proteins and hormones. (h) Sensitivity (%) as a function of PSA concentration in pure human serum media (Reproduced from [20] with permission from Wiley, 2023.)
2.2 Selectivity
Yu-Tao Li and colleagues have devised a novel approach by developing a dual needle biosensor utilizing CNT needle FETs and functionalized gates for the real-time monitoring of pH fluctuations in cerebrospinal fluid. To enhance the device's responsiveness to hydrogen ions, they modified the platinum electrode of the gate with polyaniline (PANI). Polyaniline polymers, rich in amine groups, exhibit changes in their electrical properties as the pH value fluctuates due to the protonation and deprotonation of these amine groups. In acidic solutions, PANI becomes doped with H, forming a highly conductive emeraldine salt, which, in turn, reduces the surface charge and increases surface potential [21]. Conversely, exposure to alkaline solutions neutralizes the trapped H by OH−, resulting in the reverse effect. This modification significantly enhanced the response to hydrogen ions from 27.3 to 53.7 mV/pH (pH range: 4−9). Additionally, the brain contains various ions and neurotransmitters during different activities. In their experiment, they investigated the reactivity of the dual needle biosensor with Na, K, Mg2+, DA, UA, Ach, Glu, and H. Although substances other than H were measured at significantly higher concentrations, they exhibited minimal reactivity, while H showed a substantial reaction. This confirmed the high selectivity of the dual needle biosensor. Moreover, they conducted pH measurements in rat cerebrospinal fluid using the developed sensor. By directly injecting NaH2PO4 and Na2CO3 into the rat brain to alter the pH of the cerebrospinal fluid, they observed a sharp increase in the corresponding current after injecting NaH2PO4, signifying a decrease in cerebrospinal fluid pH. Conversely, the current decreased when Na2CO3 was injected, indicating an increase in cerebrospinal fluid pH. In practical animal experiments, the biosensor successfully monitored real-time pH changes (Fig. 3) [22].
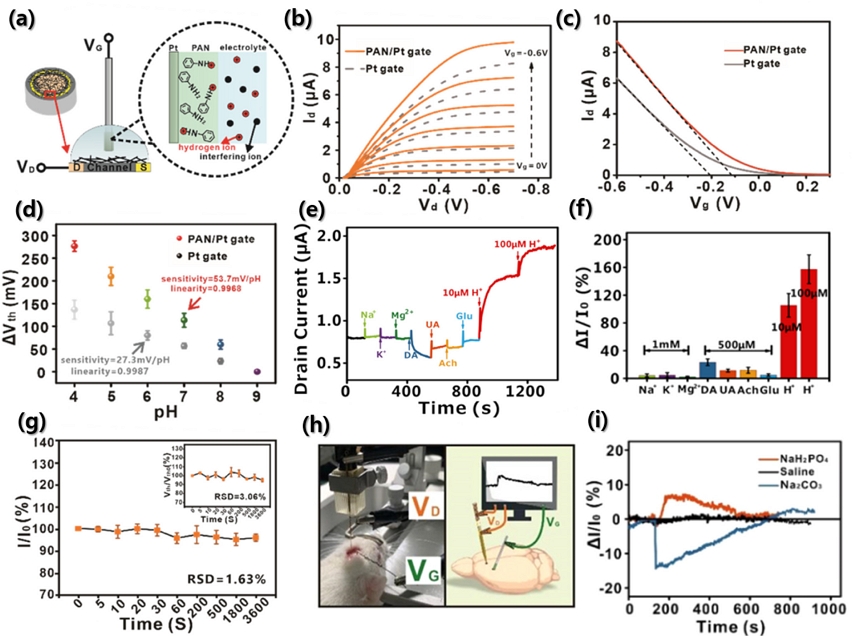
(a) Schematic of a PANI/Pt-gated CNT-FET. The conventional electrolyte gate (Pt gate) is functionalized with a polyaniline membrane. (b) Output characteristic of bare Pt-gated CNT-FET (gray dashed lines) and a PAN/Pt-gated CNT-FET (orange lines). (c) Transfer characteristic of a bare Pt-gated CNT-FET (gray line) and a PANI/Pt-gated CNT-FET (orange line). (d) Calibration curve of the change in Vth variations and pH value of bare Pt-gated (gray points) and PAN/Pt-gated (color points) CNT-FET. Vth was extracted from the linear fits (black dashed lines) of the different transfer curves. (e) Selectivity measurement of dual-needle biosensor with the addition of a series of interferents. (f) Histogram of current change rates versus various interferents and H+. (g) Corresponding Ids changes for 1 h stability measurement. (h) Schematic diagram of in vivo experiment. (i) Real-time current monitoring of pumped saline (black), NaH2PO4 (red), and Na2CO3 (blue) in rat brains using the dual-needle biosensor (Reproduced from [22], with permission form ACS publications, 2023)
2.3 Stability
Mariantonietta Parracino and her team have developed an eco-friendly biosensor based on lactate oxidase (LOX), capable of repeated use and storage at room temperature, for the dependable detection of lactic acid. The detection of lactic acid finds applications in early symptom diagnosis, such as intraabdominal sepsis and acidosis, assessing the physical condition of athletes, and evaluating the freshness and quality of food [23-28]. In their research, they fabricated the biosensor using electrospray deposition (ESD) technology, enabling a streamlined, one-step process without the need for additional material synthesis. Particularly, this approach eliminates the use of harmful chemicals, rendering it efficient and environmentally friendly. However, notably, lactate oxidase is a notably unstable enzyme, necessitating additional immobilization techniques. Despite this drawback, ESD technology offers a unique advantage by enabling the creation of sensors that can be stored and reused for extended periods, a feat not easily achieved with other immobilization technologies. Furthermore, the study compared the stability of lactic acid detection biosensors and found that those fabricated using ESD technology exhibited 100% stability over 24 consecutive measurements. Remarkably, these biosensors retained their initial characteristics even after a year. Biosensors produced via ESD technology are not only easy to process but also environmentally friendly and exceptionally stable, making them a promising choice for the commercialization of biosensors (Fig. 4) [29].
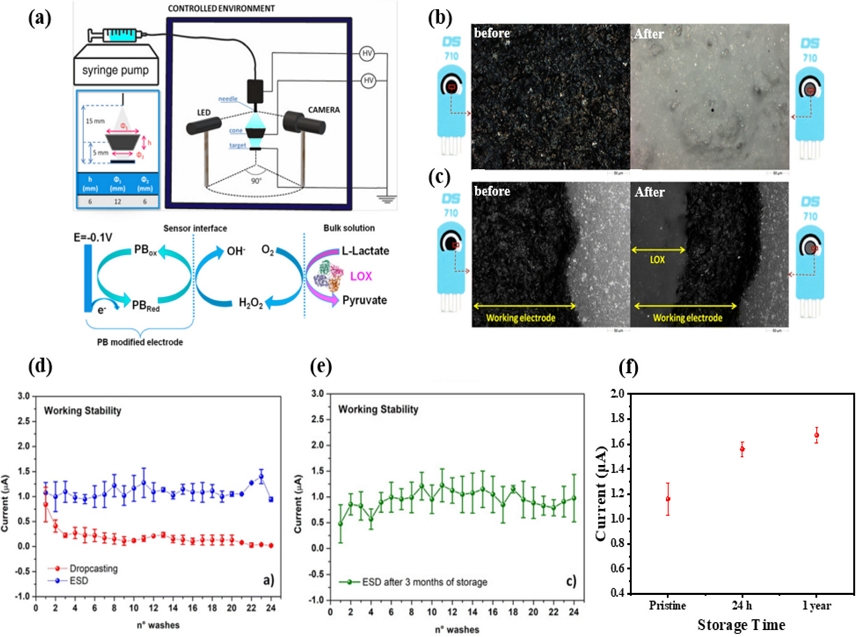
(a) Schematic of the ESD setup (top right panel) and enlarged scheme of the deposition region (top left panel) where the dimensions and the relative distance between the needle, cone, and the PB/C-SPE are depicted. Schematic of redox reactions that occur at the electrode surface during amperometric measurements (bottom panel). Before and after images of lactic acid enzyme deposition: (b) central part and (c) edge part. (d) Working stability of the e-LOX/PB/C-SPE freshly made by ESD (blue dots) and by drop-casting (red dots). (e) Working stability of the e-LOX/PB/C-SPE tested after 3 months of storage (green dots). (f) Measurement of the biosensor current after 24 h and 1 year of storage (Reproduced from [29], with permission from Royal Society of Chemistry, 2023.)
Ensuring the stability of sensor signals is of paramount importance, especially given that many biosensors operate in inherently unstable environments, necessitating their ability to function reliably despite external stimuli [30, 31]. Huanyu Cheng and his team introduced a biosensor capable of monitoring physiological information and health status using soft and deformable electronic devices. They achieved this by employing printable biphasic Ga-In (bGaIn) and self-healing hygroscopic randomly hyperbranched polymers (HRHP) in combination with a kirigami design. This innovative biosensor boasts several key features, including high conductivity (3.40 × 104S·cm-1), outstanding self-healing capabilities, over 900% elasticity, and stability under 2000 repeated tension tests. These sensors were effectively employed to provide real-time monitoring of ECG signals during physical activities and to diagnose autonomic dysfunction, increased pulmonary blood flow, and decreased cardiac blood flow. Furthermore, the flexibility of the sensor enabled it to establish closer contact with the area under measurement, enhancing the reliability of the signal (Fig. 5) [32].
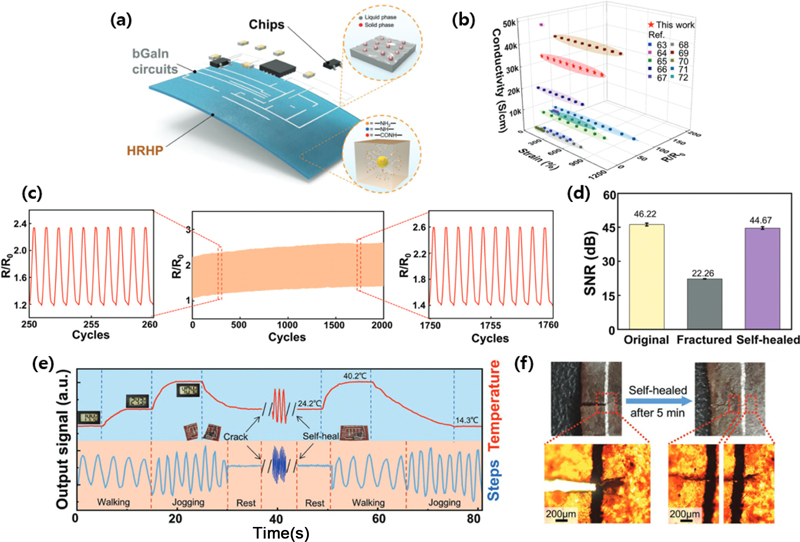
(a) Exploded view of proof-of-the-concept multifunctional electronics to monitor. (b) Comparison of initial conductivity, stretchability, and normalized resistance change at maximum strain between bGaIn from this work and other stretchable conductors. (c) The stability testing of the bGaIn traces on VHB over 2000 cycles to 300% stretching. (d) Corresponding SNR values in original, fractured, and self-healing states. (e) The signals (temperature in red and motion in blue) measured before fracture, upon fracture, and after self-healing. (f) Image showing the self-healing process of the multifunctional device. (Reproduced from [32], with permission from Wiley, 2023.)
3. APPLICATION OF BIOSENSORS
Biosensors represent the future's versatile devices with applications in disease diagnosis, monitoring, treatment, and healthcare by detecting vital signs [33, 34]. Researchers are actively developing new and improved devices to enhance their sensitivity, specificity, reliability, and biocompatibility. Bioimplantable sensors must possess key characteristics such as flexibility, stretchability, lightweight, and ultra-thin design. These features enable them to comfortably conform to the skin, accommodate continuous movement without discomfort, minimize immune reactions and biological contamination during implantation, adapt to the 3D shape of organs, obviate complex surgeries, and support wireless transmission and self-powering capabilities [35, 36].
3.1 In vitro sensors
The most studied and utilized bioelectronic devices are electrochemical biosensors based on enzyme recognition reactions. These biosensing applications depend on the remarkable substrate specificity of enzymatic reactions and reaction rates, that are proportional to concentration. Joseph Wang et al. developed a system for real-time monitoring of glucose and alcohol level in sweat and bodily fluids using biosensors. The sensor detected glucose and alcohol concentrations by immobilizing glucose oxidase (GOx) and alcohol oxidase (AOx) on the surface of Prussian blue-carbon electrodes with the aid of chitosan hydrogels. The sweat-inducing drug pilocarpine was injected into the skin to check the behavioral characteristics, and the measured results were monitored in real time through a laptop and a mobile device via Bluetooth in the sensor. Furthermore, even under repeated (120 times) bending tests at 90°, the characteristics hardly changed and the operation remained stable. Through this in vitro biosensor, the authors presented a platform that could be used to monitor the glucose levels of diabetic patients in real time and prevent drink-driving accidents in advance (Fig. 6) [37].
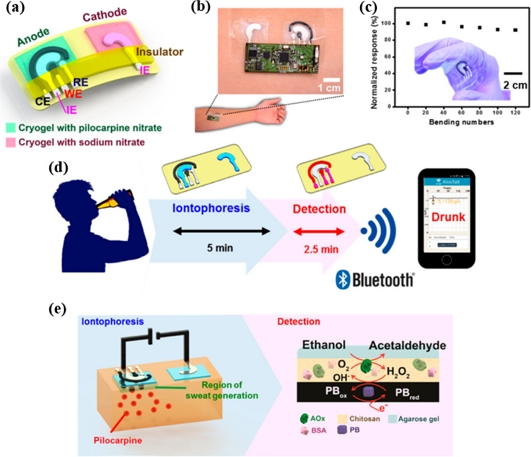
(a) Tattoo biosensor with the iontophoretic. (b) Alcohol iontophoresis tattoo sensor with integrated flexible electronics attached to a human subject. (c) Mechanical deformation test of the tattoo sensor. (d) Schematic of a wireless operation of the iontophoretic-sensing tattoo device for transdermal alcohol sensing. (e) Schematic of constituents in the iontophoretic system (left) and of the reagent layer and processes involved in the amperometry sensing of ethanol on the working electrode (right). (Reproduced from [37], with permission from ACS Publications, 2016.)
3.2 In vivo sensors
In vivo biosensing has substantially elevated healthcare standards, as in vivo biosensors enable continuous monitoring and even treatment of patient conditions. While many sensors have been developed to detect physiologically relevant analytes, displaying tremendous potential for in vivo monitoring, most of them have only been studied at the animal level. Consequently, there are limited instances of biosensors approved for human implantation. Notably, Zhou Li and colleagues designed a soft sensor using an adhesive hydrogel (AH). This soft sensor exhibits exceptional properties, enduring more than 631% tensile strain with a corresponding breaking strength of 140 kPa. It also boasts a high output of 8.3 V, long-term stability over 6000 cycles, and a high power density of 186.9 μWm−2 (Fig. 7) [38].
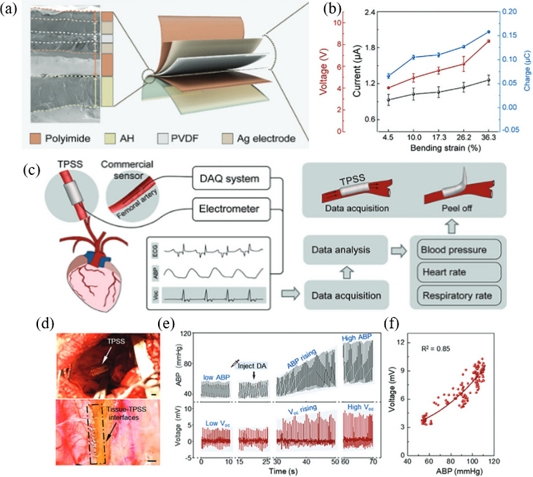
(a) SEM and explosive view of TPSS displayed the multi-layered structure with close contact between layers. (b) The Voc, Isc, and Csc of TPSS vary with different bending strains. (c) Schematic diagram of in vivo experimental test system. (d) TPSS is closely attached to the surface of the right-side internal carotid artery. (e) Blood pressure data from a commercial sensor (top) and the corresponding output signals from TPSS (down). (f) Relationship between the arterial blood pressure and the output voltage of TPSS. (Reproduced from [38], with permission from Wiley, 2023.)
4. CONCLUSIONS
The growing focus on human healthcare has spurred the development of wearable devices equipped with biosensors for continuous biomonitoring. To make these biosensors market-ready, improvements in terms of sensitivity, selectivity, biocompatibility, and flexibility are crucial. This review article introduces the fundamental attributes of biosensors, including sensitivity, selectivity and stability and delves into the latest research trends aimed at enhancing these characteristics. Furthermore, the article explores ongoing research in various applications of biosensors, such as real-time monitoring of heart rate and physical activity, blood glucose monitoring, brainwave surveillance, environmental monitoring, and real-time DNA detection, both inside and outside the human body. Although, promising results have been achieved through in vitro and animal-level in vivo testing, the application of these sensors to humans necessitates addressing performance, regulatory, and ethical considerations. Deregulation related to biosensor usage is a delicate issue, and privacy and ethical aspects must be carefully considered. As technology continues to advance, and the collection and utilization of biometric information become more widespread, regulatory issues associated with biosensors are actively discussed. From a technological perspective, extensive research is ongoing to pave the way for the commercialization of biosensors. The widespread adoption of these devices is expected to usher in transformative changes in healthcare, environmental monitoring, life sciences, food, military applications, IoT, and many other fields.
Acknowledgments
This work was supported by the 2023 Research Fund of the University of Seoul.
REFERENCES
-
Y. Ohm, C. Pan, M. J. Ford, X. Huang, J. Liao, and C. Majidi, “An electrically conductive silver–polyacrylamide–alginate hydrogel composite for soft electronics”, Nat. Electron., Vol. 4, No. 3, pp. 185-192, 2021.
[https://doi.org/10.1038/s41928-021-00545-5]

-
Q. Su, Q. Zou, Y. Li, Y. Chen, S.-Y. Teng, J.T. Kelleher, R. Nith, P. Cheng, N. Li, and W. Liu, “A stretchable and strain-unperturbed pressure sensor for motion interference–free tactile monitoring on skins”, Sci. Adv., Vol. 7, No. 48, pp. eabi4563(1)-eabi4563(9), 2021.
[https://doi.org/10.1126/sciadv.abi4563]

-
A. H. Anwer, N. Khan, M. Z. Ansari, S.-S. Baek, H. Yi, S. Kim, S. M. Noh, and C. Jeong, “Recent advances in touch sensors for flexible wearable devices”, Sensors, Vol. 22, No. 12, pp. 4460(1)-4460(21), 2022.
[https://doi.org/10.3390/s22124460]

- J. Lee, “Human Implantable Arrhythmia Monitoring Sensor with Wireless Power and Data Transmission Technique”, Biosens. Bioelectron., Vol. 1, p. 1008, 2015.
-
R. Rebelo, A. I. Barbosa, D. Caballero, I. K. Kwon, J. M. Oliveira, S. C. Kundu, R. L. Reis, and V. M. Correlo, “3D biosensors in advanced medical diagnostics of high mortality diseases”, Biosens. Bioelectron., Vol. 130, pp. 20-39, 2019.
[https://doi.org/10.1016/j.bios.2018.12.057]

-
Y. Zhang, F. Zhang, Y. Shakhsheer, J. D. Silver, A. Klinefelter, M. Nagaraju, J. Boley, J. Pandey, A. Shrivastava, E. J. Carlson, A. Wood, B. H. Calhoun, and B. P. Otis, “A Batteryless 19 µW MICS/ISM-Band Energy Harvesting Body Sensor Node SoC for ExG Applications”, IEEE J. Solid-State Circuits, Vol. 48, No. 1, pp. 199-213, 2013.
[https://doi.org/10.1109/JSSC.2012.2221217]

-
N. Yi, H. Cui, L. G. Zhang, and H. Cheng, “Integration of biological systems with electronic-mechanical assemblies”, Acta Biomater., Vol. 95, pp. 91-111, 2019.
[https://doi.org/10.1016/j.actbio.2019.04.032]

-
F. K. Shaikh and S. Zeadally, “Energy harvesting in wireless sensor networks: A Comprehensive review”, Renew. Sustain. Energy Rev., Vol. 55, pp. 1041-1054, 2016.
[https://doi.org/10.1016/j.rser.2015.11.010]

-
A. Sayad, E. Skafidas, and P. Kwan, “Magneto-Impedance Biosensor Sensitivity: Effect and Enhancement”, Sensors, Vol. 20, No. 18, pp. 5213(1)-5213(20), 2020.
[https://doi.org/10.3390/s20185213]

-
L. A. Delouise, P. M. Kou, and B. L. Miller, “Cross-Correlation of Optical Microcavity Biosensor Response with Immobilized Enzyme Activity. Insights into Biosensor Sensitivity”, Anal. Chem., Vol. 77, No. 10, pp. 3222-3230, 2005.
[https://doi.org/10.1021/ac048144+]

-
H. Sharma and R. Mutharasan, “Half Antibody Fragments Improve Biosensor Sensitivity without Loss of Selectivity”, Anal. Chem., Vol. 85, No. 4, pp. 2472-2477, 2013.
[https://doi.org/10.1021/ac3035426]

-
P. Pal, Y. Pratap, M. Gupta, and S. Kabra, “Open gate AlGaN/GaN HEMT biosensor: Sensitivity analysis and Optimization”, Superlattices Microstruct., Vol. 156, p. 106968, 2021.
[https://doi.org/10.1016/j.spmi.2021.106968]

-
Y. Wei, S. Jiang, J. Li, X. Li, K. Li, J. Li, and Z. Fang, “A biosensor material with robust mechanical properties, fatigue resistance, biocompatibility, biodegradability, and anti-freezing capabilities”, J. Mater. Chem. A, Vol. 10, No. 15, pp. 8491-8500, 2022.
[https://doi.org/10.1039/D1TA10998G]

-
S. W. Hwang, C. H. Lee, H. Cheng, J. Jeong, S. K. Kang, J. H. Kim, J. Shin, J. Yang, Z. Liu, G. A, Ameer, Y. Huangm, and J. A. Rogers, “Biodegradable Elastomers and Silicon Nanomembranes/Nanoribbons for Stretchable, Transient Electronics, and Biosensors”, Nano Lett., Vol. 15, No. 5, pp. 2801-2808, 2015.
[https://doi.org/10.1021/nl503997m]

-
H. Zhao, L. Zhang, T. Deng, and C. Li, “High-performance sensing, breathable, and biodegradable integrated wearable sweat biosensors for a wireless glucose early warning system”, J. Mater. Chem. A, Vol. 11, p. 12395, 2023.
[https://doi.org/10.1039/D3TA01084H]

-
T. P. Huynh, P. S. Sharma, M. Sosnowska, F. D. Souza, and W. Kutner, “Functionalized polythiophenes: Recognition materials for chemosensors and biosensors of superior sensitivity, selectivity, and detectivity”, Prog. Polym. Sci., Vol. 47, pp. 1-25, 2015.
[https://doi.org/10.1016/j.progpolymsci.2015.04.009]

-
J. Kim, G. V. Ramirez, A. J. Bandodkar, W. Jia, A. G. Martinez, J. Ramirez, P. Mercier, and J. Wang, “Non-invasive mouthguard biosensor for continuous salivary monitoring of metabolites”, Analyst, Vol. 139, No. 7, pp. 1632-1636, 2014.
[https://doi.org/10.1039/C3AN02359A]

-
C. S. Liu, C. X. Sun, J. Y. Tian, Z. W. Whang, H. F. Ji, Y. P. Song, S. Zhang, Z. H. Zhang, L. H. He, and M. Du, “Highly stable aluminum-based metal organic frameworks as biosensing platforms for assessment of food safety”, Biosens. Bioelectron., Vol. 91, pp. 804-810, 2017.
[https://doi.org/10.1016/j.bios.2017.01.059]

-
L. Li, X. Liu, T. Wei, K. Wang, Z. Zhao, J. Cao, and Y. Liu, “Carbon Nanotube Field-Effect Transistor Biosensor with an Enlarged Gate Area for Ultra-Sensitive Detection of a Lung Cancer Biomarker”, ACS Appl. Mater. Interfaces, Vol. 15, No. 22, pp. 27299-27306, 2023.
[https://doi.org/10.1021/acsami.3c02700]

-
A. Sen, J. Shim, A. Bala, H. Park, and S. Kim, “Boosting Sensitivity and Reliability in Field-Effect Transistor-Based Biosensors with Nanoporous MoS2 Encapsulated by Non-Planar Al2O3”, Advanced Functional Materials, Vol. 33, No. 42, pp. 2301919(1)-2301919(10), 2023.
[https://doi.org/10.1002/adfm.202301919]

-
Y. Li, Y. Mao, C. Xiao, X. Xu, and X. Li, “Flexible pH sensor based on a conductivity PANI membrane for pH monitoring”, RSC Adv., Vol. 10, No. 1, pp. 21-28, 2020.
[https://doi.org/10.1039/C9RA09188B]

-
B. Liu, S. Yu, Y. Zhou, Y. Lei, L. Tang, G. J. Zhang, and Y. T. Li, “Dual-Needle Field-Effect Transistor Biosensor for In Vivo pH Monitoring”, ACS Sens., Vol. 8, No. 7, pp. 2609-2617, 2023.
[https://doi.org/10.1021/acssensors.3c00415]

-
G. J. Kost and M. J. McQueen, “New whole blood analyzers and their impact on cardiac and critical care, Critical Reviews in Clinical Laboratory Sciences”, Crit. Rev. Clin. Lab. Sci., Vol. 30, No. 2, pp. 153-202, 1993.
[https://doi.org/10.3109/10408369309084667]

-
J. Bakker, P. Gris, M. Coffernils, R. J. Kahn, and J. L. Vincent, “Serial blood lactate levels can predict the development of multiple organ failure following septic shock”, Am. J. Surg., Vol. 171, No. 2, pp. 221-226, 1996.
[https://doi.org/10.1016/S0002-9610(97)89552-9]

-
R. Pilloton, T. N. Nwosu, and M. Mascini, “Amperometric Determination of Lactic Acid. Applications on Milk Samples”, Anal. Lett., Vol. 21, No. 5, pp. 727-740, 1988.
[https://doi.org/10.1080/00032718808070855]

-
F. Mazzi, A. Azzoni, B. Cacalieri, F. Botre, and C. Botre, “A multi-enzyme bioelectrode for the rapid determination of total lactate concentration in tomatoes, tomato juice and tomato paste”, Food Chem, Vol. 55, No. 4, pp. 413-418, 1996.
[https://doi.org/10.1016/0308-8146(95)00168-9]

-
J. Wang, “Amperometric biosensors for clinical and therapeutic drug monitoring: a review”, J. Pharm. Biomed. Anal., Vol. 19, No. 1-2, pp. 47-53, 1999.
[https://doi.org/10.1016/S0731-7085(98)00056-9]

-
A. Parra, E. Casero, L. Vazquez, F. Pariente, and E. Lorenzo, “Design and characterization of a lactate biosensor based on immobilized lactate oxidase onto gold surfaces”, Anal. Chim. Acta, Vol. 555, No. 2, pp. 308-315, 2006.
[https://doi.org/10.1016/j.aca.2005.09.025]

-
M. C. Castrovilli, V. Scognamigli, E. Tempesta, J. Chiarinelli, M. Parracino, V. Frisulli, M.T. Giardi, L. Avaldi, D. Rossi, and A. Cartoni, “Improved reuse and storage performances at room temperature of a new environmentally friendly lactate oxidase biosensor prepared by ambient electrospray immobilization”, Green Chem., Vol. 25, pp. 5257-5266, 2023.
[https://doi.org/10.1039/D3GC00494E]

-
L. Yang, N. Yi, J. Zhu, Z. Cheng, X. Yin, X. Zhang, H. Zhu, and H. Cheng, “Novel gas sensing platform based on a stretchable laser-induced graphene pattern with self-heating capabilities”, J. Mater. Chem. A, Vol. 8, No. 14, pp. 6487-6500, 2020.
[https://doi.org/10.1039/C9TA07855J]

-
L. Yang, H. Ji, C. Meng, Y. Li, G. Zheng, X. Chen, G. Niu, Y. Yan, Y. Xue, and S. Guo, “Intrinsically Breathable and Flexible No2 Gas sensors Produced by Laser Direct Writing of Self-Assembled Block Copolymers”, ACS Appl. Mater. Interfaces, Vol. 14, No. 15, pp. 17818-17825, 2022.
[https://doi.org/10.1021/acsami.2c02061]

-
L. Yang, Z. Wang, H. Wang, B. Jin, C. Meng, X. Chen, R. Li, H. Wang, M. Xin, Z. Zhao, S. Guo, J. Wu, and H. Cheng, “Self-Healing, Reconfigurable, Thermal-Switching, Transformative Electronics for Health Monitoring”, Adv. Mater., Vol. 35, No. 15, p. 2207742, 2023.
[https://doi.org/10.1002/adma.202207742]

-
R. M. Aileni, A. C. Valderrama, and R. Strungaru, “Wearable Electronics for Elderly Health Monitoring and Active Living” in Ambient Assisted Living and Enhanced Living Environment, C. Dobre, N. Garcia, G. Mastorakis, C. Mavromoustakis, and R. Goleva, Eds. Oxford, Butterworth-Heinemann, Oxford, pp. 247-269, 2017.
[https://doi.org/10.1016/B978-0-12-805195-5.00010-7]

-
M. Ghamari, B. Janko, R. S. Sherratt, W. Harwin, R. Piechockic, and C. Soltanpur, “A Survey on Wireless Body Area Networks for eHealthcare Systems in Residential Environments”, Vol. 16, No. 6, pp. 831(1)-831(33), 2016.
[https://doi.org/10.3390/s16060831]

-
V. Perumal, “U. Hashim, Advances in biosensors: Principle, architecture and applications”, J. Appl. Biomed., Vol. 12, No. 1, pp. 1-15, 2014.
[https://doi.org/10.1016/j.jab.2013.02.001]

-
S. Kumar, W. Ahlawat, R. Kumal, and N. Dilbaghi, “Graphene, carbon nanotubes, zinc oxide and gold as elite nanomaterials for fabrication of biosensors for healthcare”, Biosens Bioelectron., Vol. 70, pp. 498-503, 2015.
[https://doi.org/10.1016/j.bios.2015.03.062]

-
J. Kim, I. Jeerapan, S. Imani, T. N. Cho, A. Bandodkar, S. Cinti, P. P. Mercier, and J. Whang, “Noninvasive Alcohol Monitoring Using a Wearable Tattoo-Based Iontophoretic-Biosensing System”, ACS Sens., Vol. 1, No. 8, pp. 1011-1019, 2016.
[https://doi.org/10.1021/acssensors.6b00356]

-
C. Wang, Y. Hu, Y. Liu, Y. Shan, X. Qu, J. Xue, T. He, S. Cheng, H. Zhou, W. Liu, Z. H. Guo, W. Hua, Z. Liu, Z. Li, and C. Lee, “Tissue-Adhesive Piezoelectric Soft Sensor for In Vivo Blood Pressure Monitoring During Surgical Operations”, Adv. Funct. Mater., Vol. 33, No. 38, pp. 2303696(1)-2303696(10), 2023.
[https://doi.org/10.1002/adfm.202303696]
